Why Are My Gums Bleeding?
In this unusual time when you can’t just pop over to see us about a non-emergency dental concern, we want to keep providing you with relevant information that can help you manage issues at home. We are thrilled at the prospect of reopening on Monday, May 11. At that time, we will resume providing excellent dental care for all of our patients.
In the meantime, here is what you need to know about gums that bleed.
Why Do Gums Bleed Sometimes?
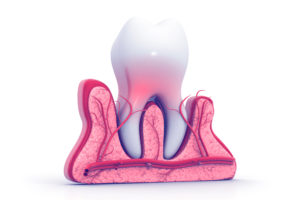
Unless you have an injury that physically cuts or tears your gum tissues, then it is safe to say that bleeding gums is the result of inflammation. The scientific term for inflammation in the gums is gingivitis.
 Inflammation is the human body’s response to injury or infection. Inflammation includes an increase in blood flow to the site of injury so that important healing cells can repair any damage. This increase in blood flow leads to swelling, redness, tenderness, a tendency to bleed, and in some cases, heat. In the gum tissues, this translates to red, puffy gums that bleed easily when you brush or floss. They might be sore, but in many cases, they are not.
Inflammation is the human body’s response to injury or infection. Inflammation includes an increase in blood flow to the site of injury so that important healing cells can repair any damage. This increase in blood flow leads to swelling, redness, tenderness, a tendency to bleed, and in some cases, heat. In the gum tissues, this translates to red, puffy gums that bleed easily when you brush or floss. They might be sore, but in many cases, they are not.
By contrast, healthy gums are generally pale pink in color and lay flat against the underlying bone.
What Causes Inflammation in the Gums?
 In the case of gingivitis, the inflammation is the result of your body responding to toxins produced by bacteria in dental plaque. Plaque contains disease-causing bacteria, food debris, and exfoliated tissue cells from the inner lining of the mouth. It is very sticky and only comes off with physical removal from brushing and flossing.
In the case of gingivitis, the inflammation is the result of your body responding to toxins produced by bacteria in dental plaque. Plaque contains disease-causing bacteria, food debris, and exfoliated tissue cells from the inner lining of the mouth. It is very sticky and only comes off with physical removal from brushing and flossing.
When you do not remove plaque from the teeth and gums, the bacteria within produce toxins, which leads to the inflammation and all that it entails (described in the previous section). The primary cause of gingivitis is always the buildup of dental plaque. There are predisposing factors that make gingivitis more likely to occur when plaque remains on the teeth.
Predisposing Factors
There are certain scenarios that make gingivitis more likely to happen. They either increase the amount of plaque that collects on the teeth, or they increase the inflammatory response to the plaque.
- Bad Oral Hygiene – This should be a no brainer. If you don’t practice good oral hygiene (brushing and flossing every day), then you are leaving dental plaque on the teeth. More plaque = more inflammation.
- Dry Mouth – People who suffer from a dry mouth, whether as a result of a prescription medication side effect or a malfunctioning salivary gland, are at a higher risk for plaque buildup. This is because saliva fights plaque and the bacteria it contains. Without saliva, you are, in effect, fighting a losing battle.
 Hormone Surges – Many women and adolescent children experience severe gingivitis as the result of large fluctuations in hormones. This typically occurs during puberty, pregnancy, and menopause. The swings in hormone levels affect the inflammatory response in the gums.
Hormone Surges – Many women and adolescent children experience severe gingivitis as the result of large fluctuations in hormones. This typically occurs during puberty, pregnancy, and menopause. The swings in hormone levels affect the inflammatory response in the gums.- Health Concerns like Diabetes and Nutritional Deficiencies – There are certain systemic medical conditions that predispose your gum tissues to inflammation, so that they “over-react” to the presence of dental plaque. These health concerns place you into a high-risk category of gum disease.
- Food Impaction – If you have a particular area in your teeth where you constantly have food being stuck during meals, you have “food impaction”. When food collects between two teeth or between the tooth and gums, it harbors bacteria and leads to inflammation.
How Do I Manage Bleeding Gums at Home until Designer Smiles Reopens?
If you or a loved one are experiencing any of the symptoms of gingivitis/bleeding gums, you should take the following steps to relieve your symptoms and slow down the progression of any gum disease.
- Brush your teeth using a gentle circular motion that touches the gums and every exposed surface of every tooth. Do this twice a day, preferably after breakfast and just before bed.
- Floss every night. Flossing is the only way to remove food debris and plaque buildup from between the teeth. Brushing alone will not cut it. If you have an area of food impaction, as described above, you may also need to floss after every meal in that area.
- Use an antiseptic mouthrinse. Avoid harsh chemicals that burn or sting. Select an alcohol-free formula, and use it as a pre-brushing rinse to break up food debris and plaque. Ask Dr. Ann and Dr. Lauren for a specific recommendation based on your unique needs and risk factors.
- Address dry mouth. If your mouth is dry, for any reason at all, you need to take steps to moisturize the inside of your mouth constantly. This involves staying well-hydrated, avoiding caffeine and alcohol, using salivary stimulants (like Xylimelts) and oral lubricants (like Biotene Dry Mouth Gel).
- Talk to your medical doctor about other potentially related health concerns or any prolonged hormone surges. You may need to work with your primary care physician to address underlying issues that contribute to gingivitis.
We Are Here for You!
We are available now to make appointments for May 11 and beyond. As always, we look forward to taking great care of you and your loved ones. If you have any urgent dental concerns before May 11, please call the office to reach our on-call dentist (Dr. Ann).