How Can a Dentist Help with my Sleep Apnea?
 That’s a great question!
That’s a great question!
Many people are confused by the fact that dentists identify signs of sleep apnea and offer treatments for it. The only part of the process dentists do not perform is the official diagnosis.
This week’s blog will explain this involvement to help you understand sleep apnea, and ways in which your dentist can help.
What is Sleep Apnea?
When we refer to sleep apnea, we are referring to the specific type known as Obstructive Sleep Apnea, or OSA. There is another form of sleep apnea called central sleep apnea, and dentists do not address that type of apnea.
Obstructive sleep apnea is a condition in which a person stops breathing for various lengths of time during sleep because of a blockage of the airway. When someone stops breathing, the oxygen levels drop in the bloodstream, and then in the brain.
Sleep apnea is a serious medical condition that can lead to a worsening of other health problems, including high blood pressure, stroke, diabetes, depression, and obesity. It also greatly impairs the quality of sleep you get each night. Your body cannot be completely healthy without good quality sleep.
Isn’t Sleep Apnea a Medical Problem? Why is my Dentist Talking about it?
Sleep apnea is a medical condition. Your dentist is talking about it for two important reasons. First, obstructive sleep apnea often leaves visible evidence inside the mouth, so your dentist could be the first one to spot your risk for it. Secondly, one of the most popular treatments for obstructive sleep apnea involves the use of an oral appliance.
As we mentioned in the introductory paragraph, the only part of the sleep apnea process for which your dentist is not responsible is the medical diagnosis. We are happy to work closely with your medical doctor or a sleep lab to obtain the necessary diagnosis. This is important when you want to use your medical insurance benefits to cover a portion of the treatment.
Dental Consequences of Sleep Apnea
Patients with obstructive sleep apnea are at risk for a few dental problems as a consequence of the lapse in breathing. If you know that you have sleep apnea, talk to Dr. Ann about how you can prevent these common consequences from developing.
Bruxism
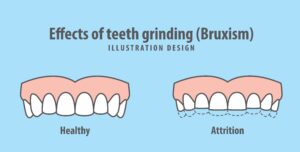 Bruxism is the scientific term we use to describe the subconscious habit of heavy teeth clenching and/or grinding of the teeth. When the brain senses a drop in oxygen levels, it sends various signals out to the body in an attempt to raise them. One of those signals is to bring the jaws together and press the lower jaw slightly forward. This motion of the jaws can physically open the airway. (If you’ve taken a CPR course, you will recognize that this is what you are doing when you pull the lower jaw out.)
Bruxism is the scientific term we use to describe the subconscious habit of heavy teeth clenching and/or grinding of the teeth. When the brain senses a drop in oxygen levels, it sends various signals out to the body in an attempt to raise them. One of those signals is to bring the jaws together and press the lower jaw slightly forward. This motion of the jaws can physically open the airway. (If you’ve taken a CPR course, you will recognize that this is what you are doing when you pull the lower jaw out.)
Untreated obstructive sleep apnea will cause heavy clenching and/or a forward grinding of the lower jaw. Your dentist can see evidence of this subconscious habit inside your mouth.
It may manifest as flattening or shortening of the teeth, small gaps developing between the upper front teeth, thickened muscles, or callousing on the cheeks and tongue. You may experience muscle pain in your cheeks and/or temples or generalized sensitivity of the teeth.
Acid Erosion
Another potential consequence of obstructive sleep apnea is acid reflux caused by negative pressure in the esophagus. The body will still attempt to breathe, expanding the ribs to draw air into the lungs. If the airway is blocked, that expansion creates a vacuum-like effect and actually pulls acid up out of the stomach into the esophagus and mouth.
This stomach acid is highly erosive and damaging to the teeth. Many people with untreated OSA show signs of acid erosion on the teeth. The acid and bruxism can have an exponential effect on each other, leading to marked erosion.
TMJ Problems
The heavy forces caused by bruxism can also lead to problems in the jaw joints. TMJ disorder manifests itself in a wide variety of ways. Some people experience pain in the jaw joints and muscles. Others have no pain, but they notice clicking or popping sounds in the joints when they speak and chew. Most damage to the TMJs is irreversible.
Dental Treatment for Sleep Apnea
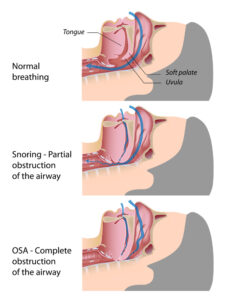 Due to the prevalence of obstructive sleep apnea, there are a variety of treatment options these patients can use to manage their condition. One important thing to understand is that sleep apnea is not ever cured. All treatments work to maintain an open airway during sleep. If you stop using the treatment, the airway will collapse again, and the condition will persist.
Due to the prevalence of obstructive sleep apnea, there are a variety of treatment options these patients can use to manage their condition. One important thing to understand is that sleep apnea is not ever cured. All treatments work to maintain an open airway during sleep. If you stop using the treatment, the airway will collapse again, and the condition will persist.
While there are several different types of dental appliances that can treat OSA, they all work in the same way. The goal of dental appliance therapy for the treatment of obstructive sleep apnea is to pull the lower jaw closed and slightly forward to physically open the airway. The appliance will connect the upper and lower jaws in order to properly align them for the best air flow. We call these appliances Mandibular Advancement Devices, or MADs.
Mandibular advancement devices are a good treatment option for patients diagnosed with mild or moderate OSA. Patients with severe sleep apnea may be able to use an oral appliance in conjunction with other treatments, like a CPAP or BiPAP machine. If you know you have sleep apnea and want more information about a dental appliance to treat it, call to schedule a visit with Dr. Ann. If you don’t know whether you have sleep apnea, but you know that your quality of sleep is terrible, ask Dr. Ann to look for signs of damage in your mouth. She can refer you to a sleep lab for testing.
More Questions about Sleep Apnea?
Call Designer Smiles today to schedule a consultation with Dr. Ann. She can answer any question you have about sleep apnea, investigate your specific situation for signs of this condition, and recommend any potential treatments that can help you. We love helping our patients protect their smiles and get better rest at night!